Medication Overuse Headache – A Call to Action

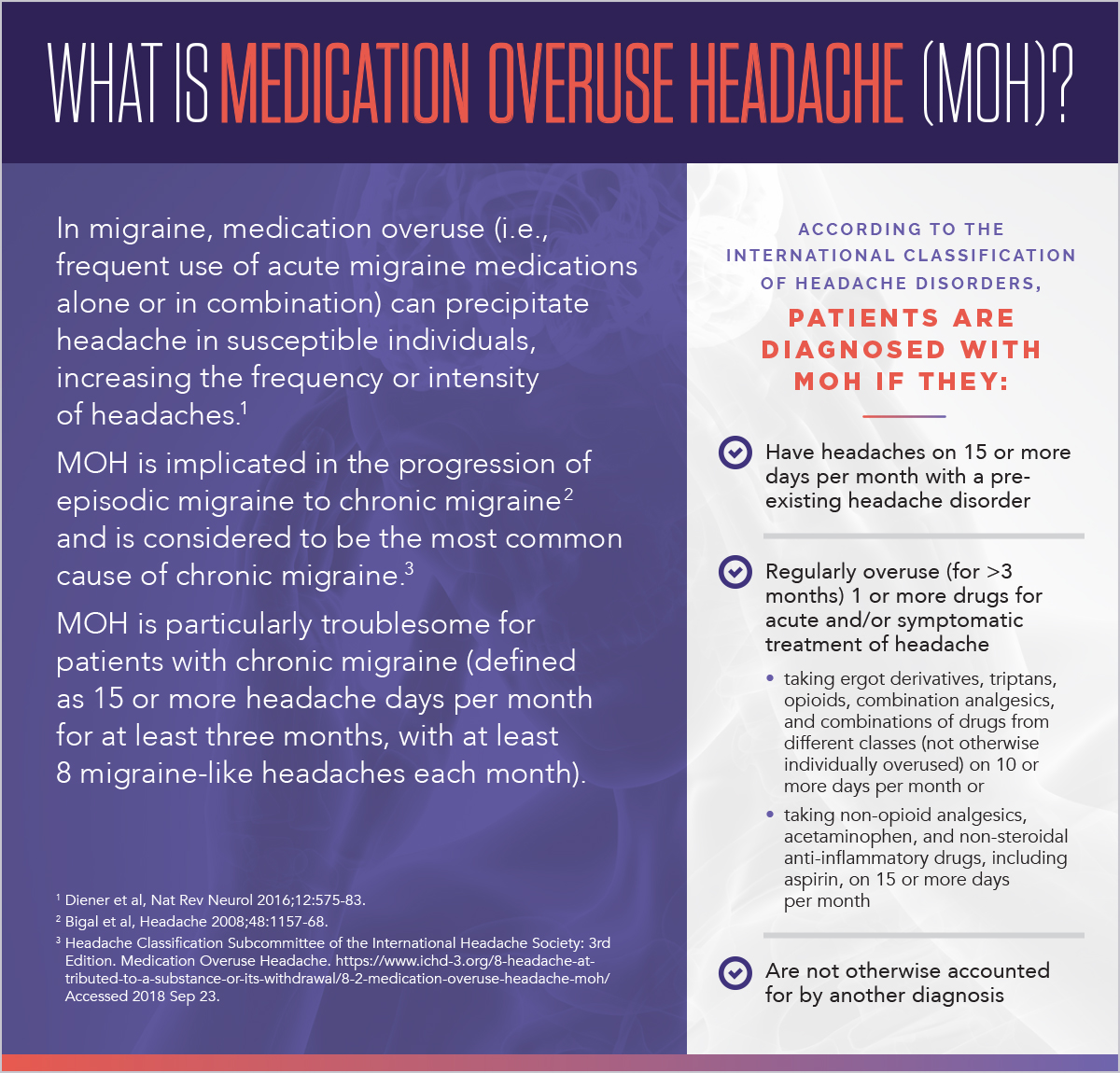
You, or someone you know, may take products like aspirin, ibuprofen, or similar over-the-counter (OTC) analgesic medications to remedy soreness after ‘weekend warrior’ athletics, to manage arthritic joint pain, or to treat tension-type headache. Anyone who consumes such analgesics or other drugs for symptomatic treatment of headache and happens to be one of the 45 million Americans with migraine or chronic tension-type headache may be at risk of medication overuse headache (MOH) (see textbox). Last year, we published a whitepaper that briefly mentioned the topic of medication overuse headache but did not adequately discuss this issue for patients with migraine. Recently, articles focusing on migraine and tension-type headache that reference medication overuse constitute a call to action for more thorough consideration of MOH.
The first of these articles, published in November 2018 and authored by an international consortium of headache specialists and epidemiologists (i.e., the Global Burden of Disease 2016 Headache Collaborators), provides insight regarding updated prevalence and disability data associated with migraine and tension type headache, following reclassification of medication overuse headache as secondary to these headache disorders. Previously, medication overuse headache was counted as a discrete neurological condition, separate from migraine and other headache types. medication overuse headache is now thought not to occur “de novo” but to be a “sequela” of migraine or tension-type headache. With the inclusion of MOH, the GBD 2016 Headache Collaborators report that these headache disorders have catapulted from 7th to 2nd place as the most frequent cause of years lived with disability (YLD) among all fatal and nonfatal diseases, with nearly 3 billion affected individuals worldwide (195 countries). When migraine is considered with tension-type headache, these two headache disorders account for >45 million YLDs and >7 million YLDs, respectively. Thus, the GBD data allow us to more fully appreciate the impact of medication overuse headache among headache disorders.
The second article, published in December 2018 and authored by scientists and clinicians managing patients with medication overuse headache (Scaratti and colleagues), describes challenges and concerns regarding medication overuse in chronic migraine. In this qualitative study, 16 patients with chronic migraine who were undergoing structured withdrawal from nonsteroidal anti-inflammatory drugs and/or triptan treatment for medication overuse headache were evaluated for personality and psychosocial characteristics. Regarding overused medications, patients showed “addictive-like” behavior, including a need to have the overused medication with them at all times, using acute medications preventively, and increasing medication use over time. These patients were also stratified according to the likelihood of relapse into chronic migraine and MOH. Frequent relapsers required two or more structured withdrawals for medication overuse headache in the course of three years. The authors observed the duration of chronic migraine was five years longer for frequent relapsers. Those who felt compelled to maintain high standards because of perceived limitations in others, using drugs to overachieve despite debilitating headaches; those who reported being “at the mercy of” headaches, exhibiting addictive behaviors related to overuse of medications; and those with symptoms suggestive of depression were also at higher risk for relapse. Based on their findings, the authors recommend that healthcare providers (HCPs) use narrative-style interviews or patient-reported outcomes to assess patients’ expectations of their disease, patients’ views of their withdrawal experiences, and patients’ perceptions of current and future social circumstances to mitigate relapse into chronic migraine and MOH. Moreover, insights obtained may be used to manage disability and co-morbidities and to design individualized management programs.
A third article, published in January 2019, is a consensus statement from the American Headache Society (AHS). In addition to providing an overview of acute and preventive therapies for patients with migraine, the statement further addresses the integration of new migraine therapies, including injectable monoclonal antibodies that target calcitonin gene-related peptide or its receptor, into clinical practice. The guidelines encourage HCPs to review patient history of medication use (whether OTC or prescription) and to assess responsiveness to acute migraine medications to minimize the risk of acute medication overuse and prevent progression to chronic migraine. Fortunately for many patients, chronic migraine can be prevented or reversed through structured withdrawal of overused and/or inappropriate medications, management of co-morbidities, patient education, adjustments in lifestyle, and addition of preventive pharmacotherapies. HCPs must be aware of these approaches and be willing to implement management strategies with their patients.
What can be done to further research the risk of MOH? The answer reasonably involves real-world data (RWD) generated at the point of care. One good source of RWD is electronic health records (EHRs). Cloud-based, bidirectional platforms such as the EHR system at Practice Fusion, a Veradigm brand, contain de-identified patient records, which may be analyzed for patterns of medication use. Such analysis may be valuable to HCPs not only for identifying drug allergies or potential drug interactions but also for specifically identifying migraine patients who are at risk of MOH, regardless of co-morbidities. For example, an individual with rheumatoid arthritis taking ibuprofen on more than 15 days each month, who also has episodic migraine, could inadvertently become a chronic ‘migrainer’ through onset of MOH. Another example would be a patient with episodic migraine who takes triptans and OTC analgesics during acute migraine attacks on 10 or more days each month. Upon reaching a critical threshold, such medication patterns may trigger support to HCPs that enables clinical decision-making regarding medication overuse or gaps in preventive therapy. The challenge occurs when HCPs don’t routinely collect detailed information regarding OTC medications or when that information only appears in notes and not in the structured fields of a patient’s electronic medical record. In such a scenario, efficient data capture and transformation could be enabled through natural language processing (NLP) or deployment of a questionnaire designed for deliberate collection of medication information into structured data fields that are accessible to ongoing analysis. Currently, Practice Fusion offers evolving NLP capability, as well as a migraine questionnaire which enables HCPs to administer MIDAS, a validated patient-reported outcome of disability. Patients and their HCPs who voluntarily use patient-reported outcome tools and structured medication history collection through EHRs may also consider engaging in real-world evidence studies (like registries or pragmatic studies) that expand our knowledge of existing medical products and contribute to the development of new drugs and biologics. Such engagement at the point of care would align with the intentions of the 21st Century Cures Act and an initiative promoted by the Framework for FDA’s Real-World Evidence Program.
For more information please contact us.